THE PARALYSIS TICK (I. holocyclus) ON HUMANS
Historical perspective
The tick bite
Allergic reactions
Tick-transmitted diseases
Paralysis or "Tick Poisoning"
Occurrence of tick poisoning in children (1999)
Removing the tick
Treatment (using the CSL anti-tick serum)
Other tick species causing illness in humans (in
Australia)
Historical perspective
"Tick fever" was mentioned in Egyptian papyrus scrolls as early as 1550 B.C. and Homer, in 850 B.C., referred to the occurrence of ticks on Odysseus' dog. Cato, Aristotle and Pliny referred to ticks as disgusting parasitic animals which were very troublesome (Obenchain and Galun, Eds, 1982).
One of the earliest Australian references to ticks as a problem in human disease is found in the journal kept by Capt William Hilton Howell for his 1824-1825 journey from Lake George to Port Phillip. In this he remarked on "the small insect called the tick, which buries itself in the flesh, and would in the end destroy either man or beast if not removed in time" (Howell, 1921, and Scott, 1921).
James Backhouse, a well-travelled quaker of the early colonial period,
gives the following account (Backhouse, 1843): At Colongatta, in Shoal Haven...district,
which, like that of Illawarra, is much more favourable for the grazing of horned
cattle than for sheep. Among the enemies of the latter in these rich, coast
lands, is the Wattle Tick, a hard flat insect of a dark colour, about the tenth
of an inch in diameter, and nearly circular, in the body; it insinuates itself
beneath the skin, and destroys, not only sheep, but sometimes foals and calves.
Paralysis of the hind quarters often precedes death in these cases. Sometimes
it occasions painful swellings, when forcibly removed from the human body, after
having fixed its achorlike head and appendages in the skin. To prevent this
inconvenience, we several times, made them let go their hold, by smearing them
over with oil, or with wet tobacco ashes.
Whilst pioneering settlers knew that ticks posed a threat to their dogs and perhaps to themselves, the Australian paralysis tick was not scientifically identified until 1899 (by Neumann). It was further studied by Nuttal and Warburton (1911). By 1921 Dodd had established a definitive link between Ixodes holocyclus and clinical disease in three dogs. He found that it took 5 to 6 days from time of attachment for clinical signs to develop, with motor paralysis being the major neurological deficit. The life cycle was studied chiefly by Ross (1924) and Oxer and Ricardo (1942) and later summarised by Seddon (1951). Ian Clunies Ross (1924) also demonstrated that a toxin produced by the tick was responsible for the paralysis and not some infective agent carried by the ticks.
The first confirmed human death due to tick poisoning in Australia was reported in 1912 (Cleland) when a large engorged tick caused flaccid paralysis in a child, progressing to asphyxiation. Headstones at the Cooktown cemetery also reveal how some human deaths were attributed to ticks.(NTPF Bulletin 1, 1999).
In the first half of the 20th century at least 20 human deaths had been attributed to the paralysis tick. Eighty percent of the victims reported in NSW between 1904 and 1945 were children aged under four years. Many cases of "infantile paralysis" (later known as poliomyelitis) may well have been misdiagnosed and actually been cases of tick paralysis (Aust. Dangerous Creatures, Readers Digest, 1991). Because of the availability of modern intensive care facilities human deaths would now be very rare. In most cases humans would be supported until the effects of the toxin subsided. The use of antitoxin (derived from dogs) is reserved for the most severe cases.
The tick bite
The bites of ticks are seldom felt at first. They can easily go unnoticed and feed for days until they reach the stage of injecting their salivary toxins. Ticks do not seem to deliberately attach in bodily recesses, rather they tend to be found in such areas because they are less likely to be brushed off. The clefts behind the ears and a hair covered scalp are common locations. They may also lodge in skin folds and body orifices such as the ears (even as deep as the ear drum), nose and vagina.
Apparently the adult female stage paralysis tick may be removed from one host and attach to another. It is therefore possible that a tick might be brought into a house on a domestic pet, scratched off from it's attachment site and reattach to a human. Under these conditions the onset of paralysis may occur within a shorter time of the (secondary) attachment than the usual 3-5 days (Moorhouse, 1981).
The tick bite initially is surrounded by an area of erythema (see picture), but this progresses over days to become a distinct and firm swelling which gradually bulges around the anterior end of the ticks body, causing it to appear as though it is embedded.
| A female half-engorged paralysis tick (Ixodes holocyclus) attached to a human arm and showing the early zone of erythema. The hypostome and chelicerae are embedded but the palps are splayed out on the surface of the skin (Moorhouse, 1981) |
In the case of attachment by an adult female it is usual for a lump to remain at the site of attachment for many weeks or even months after removal of the tick. These lumps will remain as vague irritations some 3-5 mm in diameter at the site of attachment for up to 9 months. When the tick carries the Rickettsia australis organism a characteristic eschar may form at the tick lesion as well as a more generalised macular or maculopapular red rash. Ticks carrying an Australian Borrelia organism may also cause a localised rash (see examples of erythema migrans rash below). Changes in the regional lymph nodes draining the area of attachment can also lead to the formation of chronically sensitive enlargement within the node lasting for several years, particularly those around the head and neck. It is not known whether this is due to retention of parts of the hypostome or fragments of the pedipalps or other causes. If the hypostome is examined with a hand lens after removal of the embedded tick, it is often damaged.
Allergic Reactions
Allergic reactions may be local or systemic.
which ticks
Ixodes holocyclus is the species generally responsible for allergic reactions. Whilst Haemaphysalis longicornis has also been implicated in "scrub itch" (see below), such reports are very rare and the species is unlikely to be responsible for many instances compared with Ixodes holocyclus. The ornate kangaroo tick, Amblyomma triguttatum s. l., reportedly the tick most often biting humans in Western Australia, may cause a generally mild illness (Lee, 1975: Pearce and Grove, 1987; Russell and Doggett, 1995). Argasid ticks such as Ornithodoros gurneyi (the kangaroo soft tick) found in many of the drier parts of Eastern Australia, readily bite humans, but such instances are uncommom because these areas are sparsely inhabited by humans. This tick has been associated with local reactions including inflammation, oedema, itching and susbsequent necrosis, and on occasions with severe systemic effects including giddiness, vomiting, temporary loss of vision and unconsciousness (Lee, 1975: Roberts, 1970; Russell and Doggett, 1995. Allergic-type reactions in residents on Heron Island on the Great Barrier Reef have been attributed to Ornithodoros capensis (Humphery-Smith et al, 1991b; Russell and Doggett, 1995).
which stages
Larvae
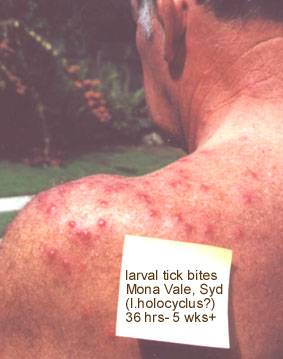
Larvae and nymphs, as well as adults are capable of causing very severe allergic reactions. Dramatic local erythema (redness) and oedema (fluid swelling) and pruritus (itch) may develop within 2-3 hours of attachment of even one larva. Frequently, a tick embedded over an eyelid will result in gross facial and neck swelling within three hours. See picture below. The person can go on to develop very severe signs of tracheopharyngeal compression within 5-6 hours after the first onset of symptoms (Jones,1991). Sometimes there is blistering.
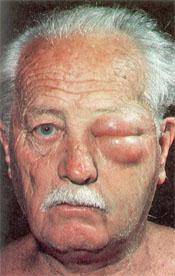 |
| Severe allergic reaction to the Australian paralysis tick Ixodes holocyclus. A larval tick was attached to the upper left eyelid for several hours only. Swelling and redness lasted for several days (Moorhouse, 1981) |
Attachment of a few larvae to a non-sensitised host provokes little or no response, even though the contact is prolonged over several days. However, towards the end of feeding some pruritus, erythema and localised odema may develop at the site of attachment. Repeated infestation with the larva, as occurs in rural and wooded suburban areas where bandicoots are common, rapidly leads to the development of hypersenstivity. Then attachment of the larvae leads to formation of intra-epidermal blebs and eventually vesicles. Finally these rupture and the larvae detach and are lost. In experimental work with the cattle tick Boophilus microplus, this occurred within 6 hours. When, as is often the case, large numbers of larvae are involved, severe allergic dermatitis may result. The maddening rash that results is commonly referred to as scrub-itch. See picture below.Outbreaks are seasonal in southeast Queensland and occur most commonly during January, February and March when larval populations are at their peak. Dermatitis is most commonly encountered in rural workers but may also result from gardening (Moorhouse, 1981). During damp summers any disturbance of taller plants - e.g. clearing lantana, can produce a shower of tick larvae.
|
|
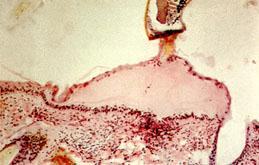
| A case of human "scrub itch". The leg of a 60 year old from Mt Tamborine, who had been bitten by multiple larval ticks of Ixodes holocyclus (Moorhouse, 1981). If you have IE 5.0+ right click on image and select the zoom in option for a closer view. | Vesicle ("blister") formation in the superficial skin layers as seen in the "scrub-itch" induced by tick larvae. The tip of the hypostome is in the upper part of the section. Microscopic view (Moorhouse, 1981). |
|
| An apparently severe, delayed and long lasting reaction to larval tick bites. At times individual lesions would swell, become itchy and then subside again despite treatment with antihistamines and topical corticosteroid. (source: Paul Ambrose via email, Qld, May 2000) |
Nymphs and Adults
Attachment of the nymphal and adult stages produce variable responses, many of which are clearly allergic in nature. Often, attachment may provoke little or no response and the patient may be quite unaware of the presence of a tick for some days (hypoaesthesia) and eventually minor itchiness may lead to its discovery. Conversely there is sometimes a locally heightened sensitivity or pain (hyperaesthesia) (Atwell and Fitzgerald, 1994). Such attachment sites are surrounded by erythema (redness) (Moorhouse, 1981).
After the tick is removed pruritus (itchiness) may recur at the site of attachment at intervals over some weeks, and a small firm lump usually forms within a day or so of the tick's removal. This again may persist for many weeks. There may be some discoloration of the area of the bite. In other cases the skin reactions may be severe with marked pruritus and considerable erythema, oedema and induration (hardening) (Moorhouse, 1981). People also report headaches (Atwell and Fitzgerald, 1994).
Tick Products
Apparently many people have experienced spectacular reactions when they have come into contact with both live and dead tick products. Having a tick simply walk over a person's hand produces in some people an intense discomfort and itching. It is not yet known what particular components of the tick body cause these allergic and hypersenstive effects. It could be a water soluble component that is excreted through the cuticular canals (see toxicology).
anaphylaxis (allergic shock)
Systemic reactions to tick bites may include headache, dizziness and malaise. Anaphylaxis has been reported in humans following contact with Ixodes. Often it occurs within a few hours of tick attachment (Moorhouse, 1981). It may also be triggered by removal of an attached female (Stone and Binnington, 1986; Stone, 1990; Stone et al, 1994). Anaphylaxis may occur after repeated exposure or even after a suspected first exposure. The result is collapse and prostration. Syncope (fainting) may also be a feature (Banfield, 1966). Individuals that develop even localised allergic reactions should avoid situations of exposure to ticks- further exposures can eventually go on to cause potentially fatal allergic shock. Such individuals should perhaps carry antihistamines and adrenaline when the risks are unavoidable. Wearing repellants such as those containing DEET may also be warranted. See Prevention.
A strange feature of these systemic reactions is that they cannot be entirely related to the frequency of contact between the person and the tick. While one tick may provoke a severe allergic response, another bite a few days later may elicit only a the most minor response. It seems possible that some reactions are not to the tick per se, but to pathogens transmitted by ticks. Quite apart from the well-known organisms such as Rickettsia sp and Coxiella sp, ticks transmit a host of protozoan and other microbes of domestic, feral and native animals, and it is probable that some allergic reactions result from their innoculation while feeding (Moorhouse, 1981).
Research on paralysis tick allergens is being conducted at the University of Technology, Sydney. Main participants are C Dorey and KW Broady. Research abstract: "The Australian paralysis tick, Ixodes holocyclus as well as causing significant veterinary problems due to the neurotoxin also causes significant human clinical problems due to allergic reactions following atachment of the tick. The reactions range from mild skin reactions [erythaema] to life-threatening anaphylaxis. Researchers have identified several major and minor allergens in whole tick extracts, salivary gland extracts and saliva. It has been demonstrated that two of the major allergens are not produced following attachment of the tick and are presumed to be involved in the early stages of tick attachment. One major allergen has been characterised through the production of a partial gene clone. Cross-reaction of tick allergens with dust mite and mosquito allergens have been identified and are being investigated. These cross-reactions may provide an explanation of the reports of severe allergic reactions to ticks on first exposure." See Dorey,C.N., Thurn,M.J. and Broady, K.W. Allergens of the Australian paralysis tick. In: Proceedings of the Sydney Allergen Group, Vol.7, 87 (1992).
Tick-transmitted Diseases
Many ticks worldwide are capable of transmitting viral, bacterial and protozoal diseases. In Australia Ixodes holocyclus is known to be capable of transmitting some of the bacterial diseases.
In Australia, Rickettsial Spotted Fever (Rickettsia australis), Flinders Island Spotted Fever (Rickettsia honei) and Australian form of Lyme Disease (Borrelia sp.) are the major concerns although Q fever (Coxiella burneti) is also a potential pathogen.
Rickettsial Spotted Fever
Incubation period is 7 to 10 days and initial symptoms are malaise, headache, fever, myalgia, stiff neck, nausea, vomiting, and mental confusion. It is apparently not uncommonly seen in tick collectors in southern Queensland. One bout of the disease seems to confer solid immunity. It is rarely fatal. There is usually an obvious eschar 2-5 mm in diameter at the bite site and a lymphadenopathy of regional lymph nodes. An eschar is present in 65% of cases . Later, between the third and fifth day (range 1-12 days after onset of symptoms), an erythematous (red) macular (spotted) or maculopapular (raised) rash develops on the trunk, and later the face, palms and soles. Diagnostic serology is available in the form of IgM and Weil-Felix tests. The disease runs it's course in two weeks or so but can be cured more quickly with antibiotics. Changes in the regional lymph nodes draining the area of attachment can also lead to the formation of chronically sensitive enlargement within the node lasting for several years, particularly those around the head and neck. Treatment is with tetracyclines and is usually rapidly effective, although rare fatalities have been recorded.
Australian Borreliosis
Whilst the offending Borrelia sp organism(s) has not been clearly characterised, a form of Australian human borreliosis does seem to occur. Incubation period ranges from 3 to 30 days after a bite from an infected tick. Often a lengthy elapsed time causes considerable confusion for diagnosticians. The clinical signs of human borreliosis in Australia are similar to the classic Lyme Disease in America (first described in the USA in 1975, isolated in 1981 ). A wide variety of tissues may be invaded, and may lead to permanent injury to joints, heart, central nervous system and other internal organs. Early recognition and treatment with antibiotics over severeal weeks can halt the disease, but delay may result in a lifetime of chronic illness and fatigue. Differential diagnosis might include Dengue fever, Malaria, Glandular Fever, Rickettsial Spotted Fever, Epidemic Poly-arthritis and Rheumatoid arthritis. Diseases similar to Lyme disease caused by related borrelia and transmitted by Ixodid ticks also occur in Europe and Japan. As yet there is no definitive test for Borreliosis in Australia because the organisms are difficult to culture and hence to identify and characterise. The Tick Diseases Research Unit (TDRU) at the Royal North Shore Hospital in Sydney, comprising specialist physicians, parasitologists, microbiologists, medical practitioners and other health workers is investigating tick-borne infections in the Sydney region.
 |
 |
These are examples of "erythema migrans" (EM) rashes as caused by the North American Lyme Disease; an Australian form of EM rash has been associated with the suspected Australian Lyme-like disease; note that considerable variation in appearance and location occurs; source: the Texas Department of Health. |
For more detailed information see Tick-Transmitted Diseases (Australia) and Vector Competence.
Paralysis or "Tick Poisoning"
In young children the first signs of toxicity may include lethargy, loss of appetite and an unsteadiness in walking, with a tendency to incoordination (ataxia). A child may sleep for unusually long periods and be dificult to rouse. Often their voices change and they they may have difficulty in focusing. Muscular weakness soon develops and the child staggers and falls. Weakness increases until the child is unable to walk. The arms become tremulous on effort and obviously weak. There is difficulty in swallowing, and the muscles of respiration become affected, leading to dilation of the nostrils, laboured respiration, cyanosis and ultimately, death. If the patient survives this period of extensive paralysis, resolution then begins, leading eventally to recovery.
In older children and in adults, the first manifestation of toxicity may be difficulty in reading. Double vision (diplopia), aversion to light (photophobia), dilation of the pupils (mydriasis) and transient squinting may occur. Darting movements of the eyes (nystagmus) or a sluggish reaction to light may be detected. Adults usually sufer from dizziness, headache and a general weakness and lethargy.
If the tick can be found and removed before its engorgement has proceeded to any considerable extent, paralysis may be limited and transient. In some patients a purely local paralysis develops.A bite behind the ear for example can produce a palsy on that side of the face lasting for some days. See picture.
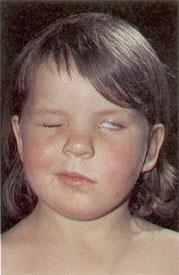 |
| A six year old girl with a left-sided Bell's Palsy. An adult female paralysis tick Ixodes holocyclus had been embedded behind the left ear for several days. The left side of the face, and the left-sided peri-ocular muscles are paralysed (Moorhouse, 1981). |
Current situation of tick poisoning in children
Some observations from Dr Rob Pitt MBBS FRACP FACEM, Director Paediatric Emergency Medicine, Mater Childrens Hospital in Brisbane (Dec 1999):
"We probably see a couple [of children with tick paralysis] a year in the Emergency Department but would only need to ventilate every second year or so. We seem to have had increased numbers in SE Qld this summer [1999]. We suspect tick paralysis in any child exhibiting unusual neurological signs because the presentation is so varied and often difficult to explain in conventional neurological terms. I have had children present with unilateral dilated pupil when the tick was between the shoulder blades. Cranial nerve palsy is the most common neurological sign. Progressive weakness starting in the legs can develop over 18 to 36 hours with clumsiness and slurred speech. Some children display bradycardia or other evidence of dysautonomia. All the severe cases with respiratory failure get 2 ampoules of antitoxin but there is seldom any immediate response. Recovery can take many weeks for these severely affected children. In population health terms, tick envenomation is a far greater medical problem for children than snake or spider bite."
Removal of the tick
For a more general discussion, pertaining to both pets and humans see Removal of ticks.
To summarise, the current principles of tick removal in Australia are: to avoid squeezing the body, to wear gloves if there is known hypersenstivity, and to first use a topical insecticide (eg pyrethroid) or repellant (eg DEET) if simple mechanical removal is not easily achievable. Squeezing the body may inject more toxin, more allergen and an infectious dose of pathogenic microbes. Worrying about removing the jaw parts (the so-called "head") is not necessary, and excessive manipulation may do more harm than good. See also the note about using topical irritants. Many recommendations for tick removal can be found worldwide. In countries where Lyme disease is a major problem it has been suggested that chemical pre-killing of the tick increases the chance of the tick regurgitating the bacteria-containing gut contents. The following examples are some of the methods described in Australian sources- the reader should draw his or her own conclusions:
TAGS (Tick Alert Group Support, Australia) gives the following recommendations (2000):
- Remove the tick as soon as possible
- Use fine-point tweezers or a tick remover
- Grasp the tick as close to the skin as possible
- Gently pull the tick straight out with steady pressure
- If you have any difficulty seek medical attention
- Wash your hands, disinfect the bite and tweezers
- CHILDREN: tell them to seek adult help for proper tick removal
- MULTIPLE TICK BITES: usually of tiny grass ticks (larval stage) are best removed if you soak for 30 minutes in a bath with 1 cup of bicarb soda
Do not try to kill the tick with methylated spirits. petroleum jelly or any other chemicals. This will cause the tick to inject more toxins.
Save the tick in a small airtight container with moist paper or a piece of grass for further examination if you become ill within a few weeks.
Tick bite can make you ill. In the short term there can be local irritation or allergy caused by injected toxin. Seek medical attention for allergic reactions or unusual symptoms. In the longer term certain individuals can suffer from tick borne infectious diseases. Tick typhus and Lyme borreliosis are the two known bacterial infections transmitted by the Paralysis Tick, Ixodes holocyclus.
Tick Typhus (or Spotted Fever, caused by Rickettsia australis). Contact your doctor if the following symptoms occur any time up to 14 days after tick bite: fever, muscle or joint pain, headache, sore throat, cough, conjunctivitis, connnfusion, intolerance to bright light, neck stiffness. There may be generalised rash up to 12 days after tick bite (it can sometimes be confused with chicken pox). At the site of the bite there may be a black scab (an eschar).
Lyme borreliosis (caused by Borrelia sp of some kind). If you experience any of the following symptoms after a few days, weeks or even months later, contact your doctor. Early infection: flu-like symptoms, headache, fever, muscle or joint pain, unusual fatigue, swollen glands, conjunctivitis. A rash may occur at the site of the bite or elsewhere,variable in shape and colour. Many people do not get a rash. Skin irritation immediately following tick bite is not necressarily a sign of infection. Chronic infection. Symptoms may include chronic fatigue, behavioural changes, severe headaches, neck problems, nerve inflammation, memory problems, eye problems, recurring rashes, intermittent or chronic disabling pain, arthritis, heart problems.
Your Pets. Dogs, cats, horses, cows etc can be infected too, often suffering similar symptoms to humans, especially arthritis.
For the latest information from TAGS write to TAGS at PO Box 95, Mona Vale, NSW 1660.
The CSL Antivenom Handbook (see White, 1995) gives the following recommendations:
- "Carefully remove the tick using alcohol to irritate it and pry it off the patient using tweezers on either side of the mouth parts. Do not hold it by the bodyand pull it off as this may leave mouth parts embedded in the skin.
- If the patient has, or develops, any symptoms of paralysis, such as gait disturbance or other muscle weakness, immediately seek medical help.
- If the patient has not had tetanus immunisation booster within the last 5 years, ensure this is given by the local doctor.
- If the wound becomes more red and painful after 24 hours seek medical help (possible secondary infection)
The CSL Tick Antivenom Product notes (MIMS Annual 1994) give the following recommendations:
- "Once found the tick's body should not be seized by forceps and pulled away as this action may cause more venom to be squeezed into the tissues of the host.
- The best way to remove the tick is to take a pair of sharp pointed scissors and, separating the points about 3 mm, press them flatly into the tissues, one on each side of the attached capitulum of the tick. Then slide the scissors gently forward so as to bring the points under the shoulder of the tick. A jerk upwards and away from the operator will almost invariably dislodge the intact tick.
- Alternatively the tick may be doused with turpentine, chloroform or some other relatively harmless volatile liquid."
A Reader's Digest publication "Australia's Dangersous Creatures" (1991) gives the following recommendations:
- "Only try to pick off a tick with your fingers if no better methods are available. Squeezing it will increase the amount of toxin it injects.
- Ideally you would kill the tick by dabbing it with a liquid repellant containing pyrethroids. Otherwise try kerosene or turpentine. Then use tweezers or small scissors to remove the animal without touching its body. Slip them gently under the head, pressing into the bite victims skin if necessary, and close them on the feeding tube. A firm steady pull will draw up the tube and the tick will come away intact."
The medical text Animal Toxins and Man - Ticks and their medical importance (see Moorhouse, 1981) gives the following recommendations:
- "Various methods of tick removal have been recommended. These range from simply pulling it off, with or without the prior application of substances such as tobacco juice, kerosene and other light oils, to surgical excision. There is no justification for surgical excision, nor is there any evidence that the various applications are of any assistance in tick removal. It is not advisable to simply grab the tick between the finger and thumb and pull, for there is at least one known case of a person entering into anaphylactic shock when this was done. The act of squeezing the tick possibly results in fluids within the tick passing back into the host. This may be sufficient to trigger anaphylactic shock. During the normal process of tick feeding, substances are certainly regurgitated from the gut back into the host as well as from the salivary glands.
- Probably the best approach to removal is to use a pair of curved forceps placed as close to the base of the proboscis of the tick as possible and apply traction. The mouthparts of some ticks will certtainly break off and be left in the skin, but this is of little or no importance. They are quite trivial and do not contain any reservoir of toxin and will eventually be sloughed off when the wound heals. However getting the mouthparts is not easywhen the tick has buried deeply into the tissues and especially where there is much oedema."
The Authorised Manual of St John Ambulance Australia (1988) gives the following recommendations:
- "if possible, apply a drop of kerosene or turpentine to kill the tick" (referes to figure showing the use of a cotton tipped applicator to do this). [web author's comment: using insect repellant (containing DEET, eg Aerogard®) or insecticide (containing a pyrethroid) are probably better]
- "if in ear, seek medical aid"
- "remove the tick by sliding the open blades of a small pair of sharp scissors or tweezers, one each side of the tick, and lever the tick outwards, being careful not to leave the mouthparts in the skin"
- "do not grasp or squeeze the tick"
- "search carefully for other ticks, particularly in the hair, behind the ears and other body crevices"
- "if the effects of the toxin persist or if the casualty is a child, seek medical aid"
- "do not use pressure immobilisation" [web author's comment: this is an interesting recommendation- no theoretical or empirical justifications for this are given]
- "note: the effects may continue for a few hours following the bite, after which the casualty usually recovers spontaneously. Antivenom is available"
A more recent St John's version says:
- kill the tick with insect repellant, kerosene or lighter fluid; reapply after 1 minute
- wait for one hour; the tick should shrink and darken and can usually be easily scraped off, if not it can be carefully pried off using small blunt curved scissors or tweezers
- a cold compress can be used to control pain
- if the effects of the toxin persist or if the casualty is a child, seek medical aid
Treatment (Use of CSL Tick Antivenom)
Composition
Antivenom is prepared from dogs hyperimmunised against the venom of Ixodes holocyclus. Each mL is capable of neutralising at least 20 mouse lethal doses.
Actions. Ixodes holocyclus is the common "bush" tick common along the entire east coast of Australia from northern Quensland to Lakes Entrance in Victoria. Fatal infestations are rare but nonfatal infestations are common, particularly among children.
Indications
Treatment of paralysis in humans caused by Ixodes holocyclus.
Precautions
As tick antivenom is heterologous to humans, untoward reactions may follow its injection. Such reactions are more likely to occur in those who have a personal or familial history of allergy or who have previously received canine antiserum. Adrenalin 1:1000 should always be kept on hand and ready for use whenever antivenom is administered.
Adverse reactions
Any of the following signs and symptoms may occur in varying degrees of severity: pallor, rapidity of pulse, general sensations of heat, itchiness or urticaria, swelling of the tongue or lips, an irritating cough, breathlessness or wheeziness, tightness in the throat or chest, nausea or vomiting, abdominal pains or discomfort, giddiness or loss of consciousness or convulsions.
Treatment of anaphylactic reactions
If a constitutional reaction should develop, the following lines of treatment should be adopted: 1) adrenaline 1:1000, give up to 0.5 mL intramuscularly if severe, repeat in 10 mins if recovery is not complete; in milder reactions adrenaline may be given subcutaneously and more slowly. 2) antihistamines may be given intramuscularly to supplement but not replace adrenaline; they are particularly useful if marked urticarial reactions develop. 3) an intravenous corticoid should be resorted to if the foregoing measures are not successful.
Serum sickness
Ths may occur after the administration of Tick Antivenom, but this is neither predictable nor preventable.
It should be noted that tick saliva also possesses allergenic properties and has caused hypersensitivity in some persons to an extreme degree. The most common allergic manifestations are urticaria and angioneurotic oedema.
Dosage and Administration
The antivenom must be given in adequate dosage if satisfactory results are to be achieved. If paralysis is evident, at least 20 mL should be given slowly by intravenous infusion. The antivenom should be diluted 1 in 10 in Hartmanns solution or normal saline.
Parenteral antihistamine cover should precede antivenom. Some clinicians also give a small subcutaneous dose of adrenaline as well as antihistamine. If symptoms persist or the patient's condition deteriorates, the dose should be repeated or increased.
Note. Tick antivenom is supplied as a sterile, freeze-dried powder. Before use the contents of the bottle and the diluent should be allowed to reach room temperature. Add the volume of sterile diluent indicated on the label (Water for Injections BP 10 mL). The powder is dissolved by rotating the bottle gently so that solution occurs without undue frothing. Caution- no antiseptic added. The reconstituted material should be used immediately and any unused solution should be discarded.
Presentation
Injection: 10 mL
Storage
Store at 2 to 8 degrees C. Do not freeze. Protect from light.
Poisons Schedule
S4
Other Tick Species causing illness in humans (in Australia)
The "indigenous tick" (Ixodes cornuatus) has been reported to cause paralysis. This pale coloured species is found along the southernmost NSW and eastern Victorian coasts and in the high country of Victoria and Tasmania (however, see notes on this distribution). It is closely related to the paralysis tick Ixodes holocyclus and differentiation from I. holocylus may be difficult. A case was described in the Medical Journal of Australia in 1986 of a three year old boy, bitten during a camping holiday, being gravely ill for nearly a week. The usual antivenom had no apparent effect. A four year old girl, bitten in northern Tasmania, was acutely ill with stomach cramps, vomiting, headache and neck pain, though she showed no sign of paralysis.
The "kangaroo tick" (Ornithodoros gurneyi) found in western NSW through Queensland to the Gulf of Carpentaria has also been reported to cause illness. Although it feeds for only a few minutes it has caused severe irritation, headaches, vomiting, temporary blindness and loss of consciousness.
The "ornate kangaroo tick" (Amblyomma triguttatum) apparently attaches itself with unusal tenacity. Sometimes the skin has to be cut to remove the tick. Lesser illnesses have been reported. Amblyomma triguttatum has been reported as causing "localised papular or papulopustular lesions" and "secondary bacterial infection with abscess formation" (Pearce and Grove,1987).
The "brown dog tick" ( see Rhipicephalus sanguineus) is a potential though infrequent parasite on humans in Australia. Local irritation is the major problem.
 |
| the brown dog tick Rhipicephalus sanguineus |
Bibliography
Atwell R and Fitzgerald M (1994) Unsolved issues in tick paralysis. Australian Veterinary Practitioner, 24(3) 156-161.
Jones DK: Tick Paralysis; in JD Stewart Memorial Course for Veterinarians: Proceedings 149: Emergency Medicine and Critical care, The Post Graduate Committee in Veterinary Science, University of Sydney, 1991.
Tick Antivenom, CSL Ltd: product information. See MIMS Annual 1994.
Australia's Dangerous Creatures, Readers Digest, 1991.
The use of turpentine, kerosene and chloroform is mentioned in the, MIMS Annual 1994 and Readers Digest articles. Other people have disputed the use of volatile agents such as kerosene and turpentine saying that these may cause the tick to disgorge stomach contents and hence inject more toxic saliva. These chemicals could also be irritating to the tick lesion and perhaps the inflammation so produced would increase the rate at which toxin was absorbed systemically [NF].
Article abstract
Brain, Volume 120, Issue 11, pp. 1975-1987: Abstract.
Clinical and neurophysiological features of tick paralysis
P. J. Grattan-Smith 1,2; J. G. Morris 2,4 ;H. M. Johnston,5 ;C.
Yiannikas 2,4 R.;
Malik,6 ;R. Russel l3 ;R. A. Ouvrier 7
The clinical and neurophysiological findings in six Australian children with generalized tick paralysis are described. Paralysis is usually caused by the mature female of the species Ixodes holocyclus. It most frequently occurs in the spring and summer months but can be seen at any time of year. Children aged 1-5 years are most commonly affected. The tick is usually found in the scalp, often behind the ear. The typical presentation is a prodrome followed by the development of an unsteady gait, and then ascending, symmetrical, flaccid paralysis. Early cranial nerve involvement is a feature, particularly the presence of both internal and external ophthalmoplegia. In contrast to the experience with North American ticks, worsening of paralysis in the 24-48 h following tick removal is common and the child must be carefully observed over this period. Death from respiratory failure was relatively common in the first half of the century and tick paralysis remains a potentially fatal condition. Respiratory support may be required for >1 week but full recovery occurs. This is slow with several weeks passing before the child can walk unaided. Anti-toxin has a role in the treatment of seriously ill children but there is a high incidence of acute allergy and serum sickness. Neurophysiological studies reveal low-amplitude compound muscle action potentials with normal motor conduction velocities, normal sensory studies and normal reponse to repetitive stimulation. The biochemical structure of the toxin of I. holocyclus has not been fully characterized but there are many clinical, neurophysiological and experimental similarities to botulinum toxin.
Abbreviations: Ach = acetylcholine; CMAP = compound muscle
action
potential
Keywords: tick paralysis; cranial nerve involvement; reduction of
compound
muscle action potentials; botulinum toxin
Departments of
1 Paediatrics and
2 Neurology, Westmead Hospital,
3 Department of Medical Entomology, University of Sydney,
Institute of
Clinical Pathology and Medical Research, Westmead Hospital,
4 Department of Neurology, Repatriation Hospital Concord,
5 Department of Neurology, Prince of Wales Children's Hospital,
6 Department of Veterinary Clinical Sciences, University of
Sydney and
7 Department of Neurology, Royal Alexandra Hospital for Children,
Sydney,
Australia
Correspondence to: Dr P. J. Grattan-Smith, Department of
Neurology, Royal
Alexandra Hospital for Children, PO Box 3515, Parramatta, NSW
2124,
Australia
The Paralysis Tick of Australia - Home
E-mail Us to report a broken link!